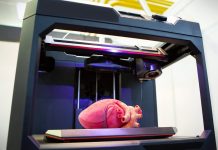
A recent breakthrough in 3D bioprinting technology has paved the way for the creation of multi-layered living skin with the potential to regenerate hair follicles.
Researchers have utilised fat tissue and its supporting structures to address injuries in rats, heralding a significant advancement in reconstructive surgery and potential treatments for hair loss in humans.
The team, led by Ibrahim T Ozbolat, a professor at Penn State specialising in engineering science, mechanics, biomedical engineering, and neurosurgery, collaborated internationally to achieve this milestone.
Collaborative innovation: from concept to patent
Their pioneering work, detailed in a paper published in Bioactive Materials on 1 March, has earned them a patent from the US Patent and Trademark Office for the bioprinting technology employed in the study.
“Reconstructive surgery to correct trauma to the face or head from injury or disease is usually imperfect, resulting in scarring or permanent hair loss,” explained Professor Ozbolat.
“With this work, we demonstrate bioprinted, full thickness skin with the potential to grow hair in rats. That’s a step closer to being able to achieve more natural-looking and aesthetically pleasing head and face reconstruction in humans,” he stressed.
Unlike previous initiatives that focused on printing thin skin layers, Ozbolat’s team has achieved a significant milestone by printing a full, living system of multiple skin layers, including the hypodermis – the bottom-most layer crucial for wound healing and hair follicle generation.
This intraoperative printing capability, allowing tissue printing during surgery, holds promise for immediate and seamless skin repair.
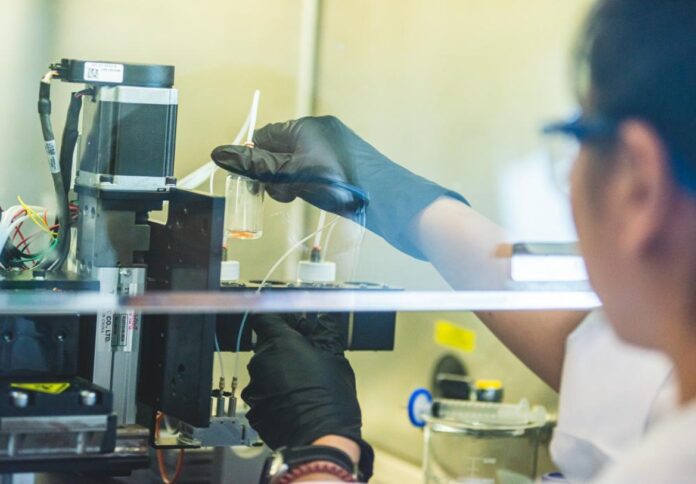
Collaborating with Dino J Ravnic, an associate professor of surgery at Penn State College of Medicine, the team sourced adipose (fat) tissue from patients undergoing surgery at Penn State Health Milton S. Hershey Medical Center.
From this tissue, they extracted extracellular matrix and stem cells, essential components for creating bioink – a material compatible with bioprinting.
“We conducted three sets of studies in rats to better understand the role of the adipose matrix, and we found the co-delivery of the matrix and stem cells was crucial to hypodermal formation,” Ozbolat noted.
He stated, “It doesn’t work effectively with just the cells or just the matrix — it has to be at the same time.”
Through experimentation in rats, the researchers observed the formation of downgrowths—the initial stage of early hair follicle development – within the printed hypodermis.
Although fat cells do not directly contribute to the cellular structure of hair follicles, they play a crucial role in their regulation and maintenance.
Bridging research and practice: the path forward
The potential applications of this technology extend beyond wound closure to encompass dermatology, hair transplants, and plastic and reconstructive surgeries.
Ozbolat said he envisions a future where this technology, in conjunction with other projects from his lab, could lead to more aesthetically pleasing outcomes in various medical procedures.
Supported by the National Institutes of Health and the Scientific and Technological Research Council of Türkiye, this groundbreaking research represents a significant step forward in the clinical translation of precisely reconstructed skin and holds promise for addressing a range of medical challenges related to skin injuries and hair loss.
This feature article was co-authored by Professor Ibrahim T Ozbolat and his research team at Penn State University.